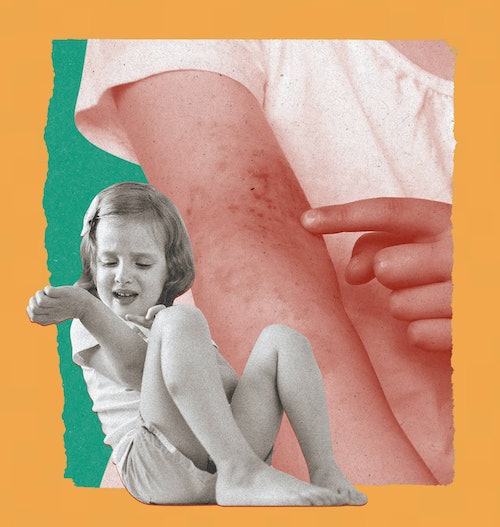
A Treatment Option For Children With Moderate-To-Severe Eczema
Intense, persistent itching. Dry, cracked rashes on the skin that can bleed, crust or ooze. Discolored skin from scabbing…
If you recognize these signs and symptoms, you or your loved ones may be dealing with moderate-to-severe eczema. This serious disease can be much more than mild itchy rashes and dry skin. Approximately 2.3 million U.S. children under the age of 18 experience this disease, yet it’s still commonly misunderstood, underestimated or dismissed as ‘easy to manage.’
For those who are less familiar: eczema is a chronic, relapsing, inflammatory skin disease that can be hereditary, with symptoms that are persistent and disruptive. Also known as ‘atopic dermatitis’ (or AD), flare-ups can be triggered by different factors including environmental allergens. It is estimated that 1 in 10 individuals will develop the disease during their lifetime, with prevalence peaking in early childhood.
It’s not easy to watch your little one live with moderate-to-severe eczema. On one end, just know it’s nothing you’re doing that is making the disease present. “One of the most common myths about eczema is that your child is doing something or you’re doing something to cause their eczema to happen,” says Dr. Marc Serota, MD, a triple board-certified doctor of dermatology, pediatrics, and allergy, asthma, and immunology. “Especially foods. People think that if I just cut out this food for my diet, my eczema will get better. In general, you’re not doing something to cause your child to have eczema, and you can’t remove something to completely take it away.”
In recent years, additional treatments have been approved which have opened up more options for managing eczema in children.
In partnership with Sanofi and Regeneron, we spoke to Dr. Serota to break down things you should know about a specific treatment option for moderate-to-severe eczema in children. Below, we share his answers to questions about the disease and an available treatment.
1. What exactly is moderate-to-severe eczema, and what does it look like?
Eczema is a chronic skin disease caused, in part, by an individual having an immune system that overreacts to allergens and irritants, resulting in inflammation that causes skin to itch.
“Moderate-to-severe eczema typically presents as rashes that are pink or red for lighter skin tones, and hyperpigmented for darker-skinned individuals,” Dr. Serota explains. “The rash is accompanied by dry, itchy skin, and can usually be found in folds of the skin, — like the crease of your elbows or the back of your knees. It can also present on the face, hands, and ankles. Due to the nature of the disease, it doesn’t always look the same every day and can also present differently in different children.”
To get the best clinical picture possible, Dr. Serota asks his patients to describe their day-to-day ‘itch score’, a rating that’s used for patients to express itch severity, during appointments so he can better understand how their disease is affecting them.
2. When should you consult a dermatologist about your child’s eczema symptoms?
Dr. Serota recommends consulting with an eczema specialist, such as a dermatologist or allergist, as soon as your child begins exhibiting symptoms.
“You don’t always know the severity of their symptoms — how intense the itch and irritation is throughout the day while they’re home or at school, or if they are scratching their skin throughout the night, until you assess it,” Dr. Serota explains. “It’s similar to intervening with hearing aids, or glasses — when children have health conditions such as eczema, it’s really something you want to address early on.”
3. What are biologics for moderate-to-severe eczema, and how are they different from other treatments?
A biologic is a drug derived biologically, or from living organisms. Biologics target specific parts of the immune system involved in the disease. Because of their size and the unique way they are made, most biologics are delivered as an injection. In the case of eczema, there is one biologic approved for use in children.
4. What is DUPIXENT (dupilumab)?
Dupixent® (dupilumab), is a prescription medicine used to treat people 6 months of age or older with moderate-to-severe eczema that is not well controlled with prescription therapies used on the skin (topical), or who cannot use topical therapies. People shouldn’t use Dupixent if they are allergic to it or its ingredients. Serious side effects include allergic reactions that can sometimes be severe, eye problems and joint aches and pain. Please see Important Safety Information below.
It is the only biologic eczema treatment approved for patients as young as 6 months of age. It helps block key source of inflammation inside the body, which can cause eczema.
Dupixent is not a steroid or an immunosuppressant.
Of the approximately 2.3 million children under 18 with moderate-to-severe eczema, an estimated 75,000 young children (age 6 months – 5 years) remain uncontrolled despite being treated with topical prescription therapies.
“When Dupixent was first approved for children, I was excited about the idea of patients having another treatment option available,” Dr. Serota explains. “When considering if Dupixent could be right for your child, it’s important to discuss the potential side effects as well as the benefits.” Before starting Dupixent, parents should discuss their children’s medical conditions and other medicines they are taking with a healthcare provider.
5. How effective is Dupixent?
Clinical trials have shown that Dupixent may help improve signs and symptoms of uncontrolled moderate-to-severe eczema for children as young as six months. In a clinical trial of young children (6 months to 5 years of age) at 16 weeks: 28% on Dupixent plus a topical corticosteroid (TCS) saw clear or almost clear skin compared with 4% on TCS only, and 48% of young children on Dupixent plus TCS had less itch compared with 9% on TCS only — individual results may vary. Patients who are deemed appropriate candidates for Dupixent can get their first dose administered by their healthcare provider.
The most common side effects include injection site reactions, eye and eyelid inflammation, including redness, swelling, and itching, sometimes with blurred vision, cold sores in your mouth or on your lips, and high count of a certain white blood cell (eosinophilia).
6. What else should parents know about Dupixent?
“Dupixent has impacted the treatment landscape of moderate-to-severe eczema,” Dr. Serota says. “If your child is affected by moderate-to-severe eczema that is not well controlled with prescription topicals, talk to your doctor about possible treatment options, like Dupixent, to see if it could be right for them.”
To learn more about Dupixent (dupilumab) and access the full Prescribing Information, visit www.dupixent.com/AtopicDermatitis/.
IMPORTANT SAFETY INFORMATION & INDICATION
Do not use if you are allergic to dupilumab or to any of the ingredients in DUPIXENT®.
Before using DUPIXENT, tell your healthcare provider about all your medical conditions, including if you:
– have eye problems.
– have a parasitic (helminth) infection.
– are scheduled to receive any vaccinations. You should not receive a “live vaccine” right before and during treatment with DUPIXENT.
– are pregnant or plan to become pregnant. It is not known whether DUPIXENT will harm your unborn baby.
– A pregnancy registry for women who take DUPIXENT during pregnancy collects information about the health of you and your baby. To enroll or get more information call 1-877-311-8972 or go to https://mothertobaby.org/ongoing-study/dupixent/.
– are breastfeeding or plan to breastfeed. It is not known whether DUPIXENT passes into your breast milk.
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements.
Especially tell your healthcare provider if you are taking oral, topical or inhaled corticosteroid medicines or if you have atopic dermatitis and asthma and use an asthma medicine. Do not change or stop your corticosteroid medicine or other asthma medicine without talking to your healthcare provider. This may cause other symptoms that were controlled by the corticosteroid medicine or other asthma medicine to come back.
DUPIXENT can cause serious side effects, including:
– Allergic reactions. DUPIXENT can cause allergic reactions that can sometimes be severe. Stop using DUPIXENT and tell your healthcare provider or get emergency help right away if you get any of the following signs or symptoms: breathing problems or wheezing, swelling of the face, lips, mouth, tongue, or throat, fainting, dizziness, feeling lightheaded, fast pulse, fever, hives, joint pain, general ill feeling, itching, skin rash, swollen lymph nodes, nausea or vomiting, or cramps in your stomach-area.
– Eye problems. Tell your healthcare provider if you have any new or worsening eye problems, including eye pain or changes in vision, such as blurred vision. Your healthcare provider may send you to an ophthalmologist for an eye exam if needed.
– Joint aches and pain. Some people who use DUPIXENT have had trouble walking or moving due to their joint symptoms, and in some cases needed to be hospitalized. Tell your healthcare provider about any new or worsening joint symptoms. Your healthcare provider may stop DUPIXENT if you develop joint symptoms.
The most common side effects in patients with eczema include injection site reactions, eye and eyelid inflammation, including redness, swelling, and itching, sometimes with blurred vision, cold sores in your mouth or on your lips, and high count of a certain white blood cell (eosinophilia).
Tell your healthcare provider if you have any side effect that bothers you or that does not go away. These are not all the possible side effects of DUPIXENT. Call your doctor for medical advice about side effects. You are encouraged to report negative side effects of prescription drugs to the FDA. Visit www.fda.gov/medwatch or call 1-800-FDA-1088.
Use DUPIXENT exactly as prescribed by your healthcare provider. It’s an injection given under the skin (subcutaneous injection). Your healthcare provider will decide if you or your caregiver can inject DUPIXENT. Do not try to prepare and inject DUPIXENT until you or your caregiver have been trained by your healthcare provider. In children 12 years of age and older, it’s recommended DUPIXENT be administered by or under supervision of an adult. In children 6 months to less than 12 years of age, DUPIXENT should be given by a caregiver.
INDICATION
DUPIXENT is a prescription medicine used to treat adults and children 6 months of age and older with moderate-to-severe eczema (atopic dermatitis or AD) that is not well controlled with prescription therapies used.
Click here for full Prescribing Information including Patient Information.
DUP.23.06.0089